Being an anxious person, I wondered if I could get an ulcer from my emotions alone, and I directly wondered if fasting could impact peptic or stomach ulcers in any way. Helping it or maybe even worsening it.
Fasting will not help an ulcer. An ulcer is not caused by bad eating habits or emotions like stress or anxiety. It is caused either by a common bacteria (H. pylori) or by certain painkillers like aspirin or ibuprofen. Also, smoking or drinking can make you more likely to get an ulcer. Fasting with an ulcer could reveal quite hazardous.
That’s not all I found out. I dug deeper and tried to find out what exactly would be the effects of fasting with an ulcer. How do an ulcer form and what anxiety and stress can really do to the stomach and digestive system?
What effects can fasting have on a stomach ulcer
Let’s first take a deeper look into what types of ulcers there are, how and why they form and what are the diet recommendations.
An ulcer is defined by a painful sore or wound that heals slowly and can recur. It can appear anywhere in your body, some known ulcers include:
- mouth ulcer
- genital ulcer
- arterial ulcer
- venous ulcer
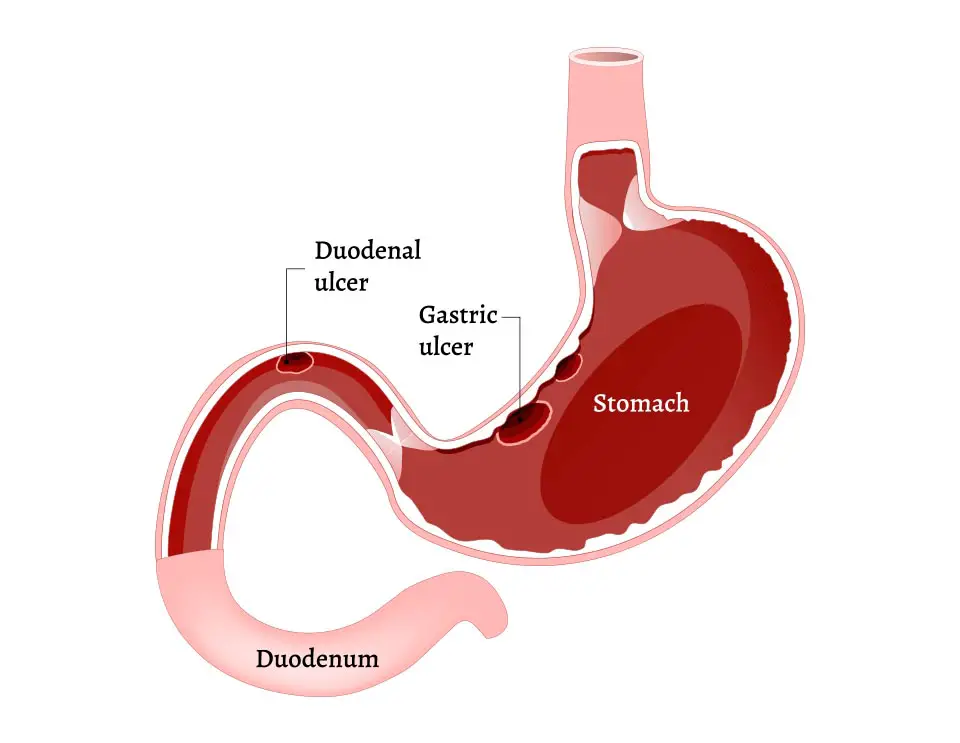
The most widely known type of ulcer though is called a peptic ulcer. This type of ulcer divides into three groups:
- Gastric ulcer, which is the one I’m mostly referring to. This one develops inside the stomach linings
- Duodenal ulcer which develops in the small intestine called the duodenum
- Oesophageal ulcer developing inside the esophagus
These types of ulcers mostly develop from digestive juices damaging the wall and linings of the organ. Those damages form sore wounds that are called ulcers.
When the lining becomes too thin or your stomach produces too much acid, your digestive system will feel it. There are two causes of inflammations leading to a peptic ulcer, bacteria or medication.
The Helicobacter pylori bacteria, also known as H. pylori for short, is a common bacteria. Almost half of the people on the planet carries the bacteria. But in most cases, people infected do not get an ulcer.
But sometimes the bacteria can raise the amount of acid in your stomach, damaging and breaking down the protective mucous lining and irritate the digestive tract. In that case, your doctor will most likely prescribe antibiotics to fight the infection and the bacteria, as well as antacids to fight stomach acid.
Medication could also be the cause of an ulcer. Prolonged exposure to certain types of painkillers, like aspirin, or even other nonsteroidal anti-inflammatory drugs (NSAID) like ibuprofen or naproxen is also a known cause for peptic ulcer.
NSAID can block your body from making the necessary chemical that helps protect the linings of your stomach and small intestine from the acid produced by your digestive system.
Of course, if medication is the cause of the ulcer, you should reduce it or stop taking them if it becomes too severe (and if you’re in a position where you can do so). You could also try to switch to another type of painkiller.
Your doctor might give you antacids or prescribe medicine to lessen the amount of acid your body makes.
As with lots of diseases or disorders, the recommended diet when you have a peptic ulcer is … a healthy one. Whole grain, fruits, vegetables. You should eat vitamin-rich meals, especially A and C, to help your body cure itself. Of course, you should also eat food with probiotics like yogurt, kimchi, miso, aged cheese, sauerkraut, etc.
Foods you should avoid include, logically, spicy food, chocolate, coffee and any acidic food like lemon or tomatoes.
It’s also widely recommended not to smoke. Smoke can make you more vulnerable to ulcers in the first place as it may interfere with the lining of the stomach and cause the production of more stomach acid.
Same thing with alcohol which irritates or even erodes the mucous lining in your stomach and intestines. This could cause inflammation and bleeding.
Stress and anxiety, which I spoke about at the beginning of this article, don’t cause peptic ulcer but it could worsen it. This could amplify acidity in the stomach and acid reflux, based on some assumptions made in certain studies.
Now I’ll get to the point: what about fasting?
A study was made in 1996 on 23 patients with peptic ulcer, engaging in Ramadan. They had several types of peptic ulcer, and different treatments. They did endoscopies before and after Ramadan and where compared against none fasting patients with the same condition.
They concluded:
In conclusion, we inferred that Ramadan fasting may prove hazardous in patients with peptic ulcer disease in general and with active chronic ulcers in particular, although the fact that only 23 patients volunteered for this study, of whom 5 were drug defaulters, is a limitation.
As you can see, no clear answer about the actual effect of fasting after the experiment. Some of them bled during the fast, but nothing seems to implicate fasting as the cause.
The thing is, fasting may slow down, or even stop, the digestive system, it may help rebuild gut flora, but ulcers are another beast, and what actually has an impact on them is stomach acid.
Does fasting have any effect on stomach acid you might ask?
Yes, it might. Sometimes fasting can cause acid reflux, which comes from acid indigestion also called dyspepsia. I haven’t found a study linking fasting and dyspepsia, most of the time, eating too much would be a greater cause of acid indigestion rather than not eating at all.
But acid reflux and acid indigestion seem to be experienced by many during fasting. Also, it seems like on prolonged fast the mucus layer covering your stomach walls grows thinner. That’s one of the reasons for eating really light and water-dense food after a long fast, to avoid producing too much stomach acid.
I myself experienced this on the first and second day of a fast mostly, I always associated this with the body getting rid of the toxins. It might be linked to that though.
But the acidity you’re experiencing at the beginning of a fast is generally directly linked to what you had to eat or drink before (carb or fat-rich food, alcohol, cigarette, etc.).
Should you fast with a peptic ulcer
As with any condition or disease, I would say you better not. Nothing proves fasting would be bad for you. But it’s commonly known that while certain foods can worsen ulcers, some can hugely relieve the pains.
I would say talk to your doctor about it. It’s a phrase I find difficult to write because most practitioners will advise against fasting in most cases anyway. Otherwise, we wouldn’t have such an epidemic of obesity and diabetes, wouldn’t we?
But in that specific case, I’m not a physician and I won’t be advising you to try fasting with such a heavy condition. You might also be treating the ulcer with some medication and most of the time, they require you actually eating to avoid acidity and other complications.
Furthermore, I haven’t found evidence leading to think that fasting could help improve your condition or even be sustainable in that case, I’ll go with the safe bet: stick to what you know and what doctors say.
Precautions when fasting with peptic ulcer
If you really want to try fasting with a peptic ulcer, then you might try and implement one or two of these good practices to help reduce stomach acidity, acid ingestion, and acid reflux during the first days of fasting.
- Drinking warm water could help settle the stomach better than cold water
- Drink water in small quantities. Do not get your belly full of water, since your stomach might think it’s full and could produce stomach acids to digest its content
- Avoid coffee, black tea or adding lemon juice, even in small amounts, to your water
- Of course, avoid cigarette at all cost
On a prolonged fast, you should take every precaution you can. When intermittent fasting, the risk of acid ingestion is far less important, but still.
After 4 to 5 days on a prolonged fast stomach acidity should decrease and this shouldn’t be too much of a problem anymore.
Related questions
Can fasting cause stomach ulcers? No. It might not help, but it’s not by any case known to be a cause or a worsening effect on ulcers, like alcohol or cigarettes.
How to know if you have H. pylori bacteria? There are no symptoms to indicate you’re infected with the bacteria. Even if you are, it might never result in getting an ulcer. If you’re suffering acute abdominal pains, especially on an empty stomach, this could mean you have a peptic ulcer and it might be caused by the bacteria.

